Blog post
Diabetic retinopathy and your eyes
How does diabetes affect the eyes?
Diabetes is a condition that causes blood glucose (sugar) levels to become too high.
High blood glucose and high blood pressure (more common in those living with diabetes) can damage blood vessels. The blood vessels in the eyes are very important as they supply blood to the light-sensitive retina.
When these blood vessels are damaged, the retina cannot get the blood supply it needs, and so cannot work as it should. This leads to diabetic retinopathy.
High blood glucose can also increase your risk of developing other eye conditions such as cataracts and glaucoma.

Can an eye test detect diabetes?
An Optician may be able to detect diabetes in an eye test.
They will be able to spot abnormalities in arteries and veins in the eyes which are a sign of conditions like diabetes, high blood pressure, and high cholesterol.
Did you know that the eyes are the only place in the body where we can see veins and arteries without invasive procedures?
Read more about what can be detected at an eye test
Do diabetics get free eye tests?
Yes, people with diabetes are entitled to free eye tests.
And if you’d rather not go out for an eye test, our mobile opticians here at OutsideClinic can come and see you in the comfort of your own home.
Do diabetics get free eye tests?
Yes, people with diabetes are entitled to free eye tests.
And if you’d rather not go out for an eye test, our mobile opticians here at OutsideClinic can come and see you in the comfort of your own home.
What is a diabetic eye screening?
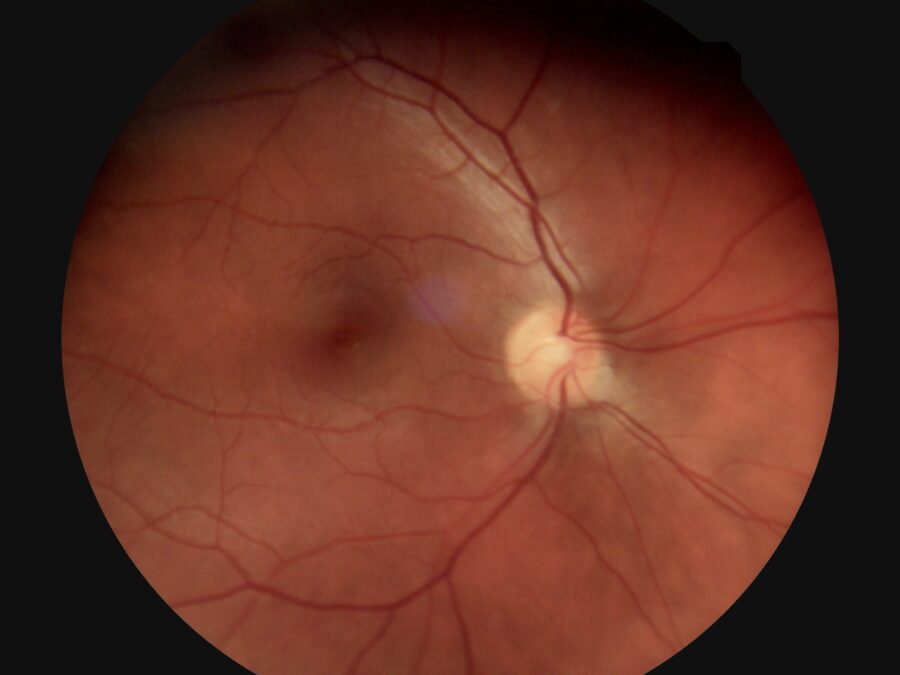
People with diabetes need to have both retinas examined. In this eye examination, the Optician checking your eyes uses an ophthalmoscope to view the retina.
First, they may dilate (widen) the pupils using special eye drops to get a clear view of the retina.
The drops used to dilate your pupils can sting a little. Your eyes will also be sensitive to bright light for a while, so wearing sunglasses may help.
If you find your vision is affected, you should avoid driving for a few hours afterwards.
What is diabetic retinopathy?
Diabetic retinopathy is a condition which affects the blood vessels in the retina (the ‘seeing’ part of the eye), causing them to become blocked, leak or grow haphazardly. This may affect the way you see things.
The condition can affect anyone with type 1 or 2 diabetes, whether they’re being treated with insulin, tablets, or diet.
Three stages of diabetic retinopathy
There are three main stages of diabetic retinopathy which are graded by how serious the condition is.
Stage 1: Background diabetic retinopathy
In the first stage, blood vessels in the retina are only very mildly affected. They may bulge slightly, leak blood or fluid but your vision will probably remain normal.
Stage 2: Pre-proliferative retinopathy
This is where more severe and widespread changes are seen in the retina, including bleeding into the retina.
At this stage there's a high risk that your vision could eventually be affected and you'll usually be advised to have more frequent screening appointments every 3, 6, 9 or 12 months to monitor your eyes.
Stage 3: Proliferative diabetic retinopathy
As the eye condition progresses this can sometimes lead to blood vessels in the retina becoming blocked.
The eye will try to repair itself by forming new blood vessels, although these vessels are weak and can easily bleed, causing scar tissue to form may lead to retinal detachment.
If a retinal detachment occurs this may cause a sudden and severe loss of vision. If untreated total loss of vision could occur with proliferative diabetic retinopathy.
Signs of diabetic retinopathy
Generally, retinopathy has no obvious symptoms until it is well advanced.
However once retinopathy starts to progress, some of the first symptoms you may experience include:
- Black spots or gaps in vision
- Gradual or sudden loss of vision
- Eye floaters
- Blurred or patchy vision
- Red and bloodshot eyes
- Eye pain
Individuals who experience these symptoms should seek advice from an Optician of their GP.

Can I drive with diabetic retinopathy?
Whether you can drive with diabetic retinopathy largely depends on how much your vision is affected.
In the early stages, diabetic retinopathy may not significantly affect your ability to drive. However, as it progresses, it can result in black spots or gaps in vision, gradual or sudden loss of vision, eye floaters, or blurred or patchy vision, all of which can make driving unsafe.
If you have diabetic retinopathy and are concerned about your ability to drive, it is important to discuss this with your Optician.

What foods help with diabetic retinopathy?
A healthy balanced diet will help to keep your blood sugar under control which is important in stopping retinopathy from getting worse.
It’s best to avoid eating lots of sugary foods and stick to whole foods, such as lean proteins, non-starchy vegetables and whole grains.
Can diabetic retinopathy be reversed?
Diabetic retinopathy can't be completely reversed, but its progression can be slowed or even halted if it’s detected early on.
Treatments for diabetic retinopathy are primarily aimed at preventing further progression or addressing complications rather than reversing the damage.
What is the treatment for retinopathy?
The most important way to stop diabetic retinopathy worsening is by controlling your blood sugar, blood pressure, and cholesterol levels and taking diabetes medication as prescribed.
Diabetic retinopathy can also be treated with laser treatment. A laser is used to stabilise the retina and the leaking blood vessels. This treatment can prevent further sight loss however, it will not make it better.
There are also overnight eye masks available, called Noctura 400, which have been developed for the treatment and prevention of diabetic retinopathy and diabetic macular oedema. The masks are a simple, non-invasive, home-based solution which are comfortable and easy to use.
The Noctura 400 works by producing a specific wavelength of light which illuminates the retina and reduces the likelihood of more leaky blood vessels being formed. This can be used at an earlier stage or in parallel with the standard treatments and may reduce the need for or the frequency of the other interventions, but always consult with your Ophthalmologist before changing your treatment plan.

How to prevent eye damage from diabetes
The good news is that sight loss from diabetes is preventable as long as you are doing all you can to protect your sight. Try these simple steps:
1. Get your eyes tested annually
Don’t wait until you notice a change in your vision. Retinopathy often has no symptoms until it is well advanced, and by this time treatment is more difficult.
2. Know your blood glucose levels
If your blood sugar is consistently high, you face a higher risk of diabetic retinopathy and other eye conditions. Your healthcare team should help you set target blood sugar levels and show you how to check them at home. The closer you can keep to your target blood glucose levels, the lower your risk of developing problems with your sight.
3. Keep your blood pressure and cholesterol under control
If these are high, they can also damage or block the blood vessels in your eyes and damage your sight. Your GP should check these levels as part of your annual review.
4. Eat healthily
This can help to keep your blood glucose, blood pressure and cholesterol levels under control. Choose foods that are lower in calories, sugar, and saturated fat. Include plenty of fruits, vegetables, beans, whole grains, lean meats, fish and non-fat or low-fat dairy products in your diet.
5. Exercise regularly
This can lower your blood sugar, blood pressure and cholesterol which in return will help to protect again diabetic eye conditions.
6. Quit (or don’t start) smoking
Smoking damages your blood vessels, which combined with diabetes, greatly increases your risk or developing diabetic eye conditions. If you are a smoker, speak to your GP about help and support for quitting.