Blog post
A guide to glaucoma: what is it, symptoms, prevention
Did you know that glaucoma is one of the most common age-related eye conditions?
The most common type of glaucoma affects about 1% of people aged 40, about 3% of people aged 60, and about 8% of people aged 80 years.
As we age, maintaining our independence and quality of life becomes even more important. So, if you are over 40, or have a loved one who is, it is important to be aware of the risks of glaucoma and take steps to protect your vision.

What is glaucoma?
Glaucoma is the group of eye conditions that damage the optic nerve.
To function properly, the human eyeball requires a certain amount of internal pressure, which is provided by a flow of liquid. Too much or too little pressure can cause damage to the optic nerve at the back of the eye. The optic nerve is the part of the eye that sends signals from the retina to the brain.
There are several different types of glaucoma including angle closure, secondary, and developmental, but the most common is called chronic open angle glaucoma.
What are the symptoms of glaucoma and how is it diagnosed?
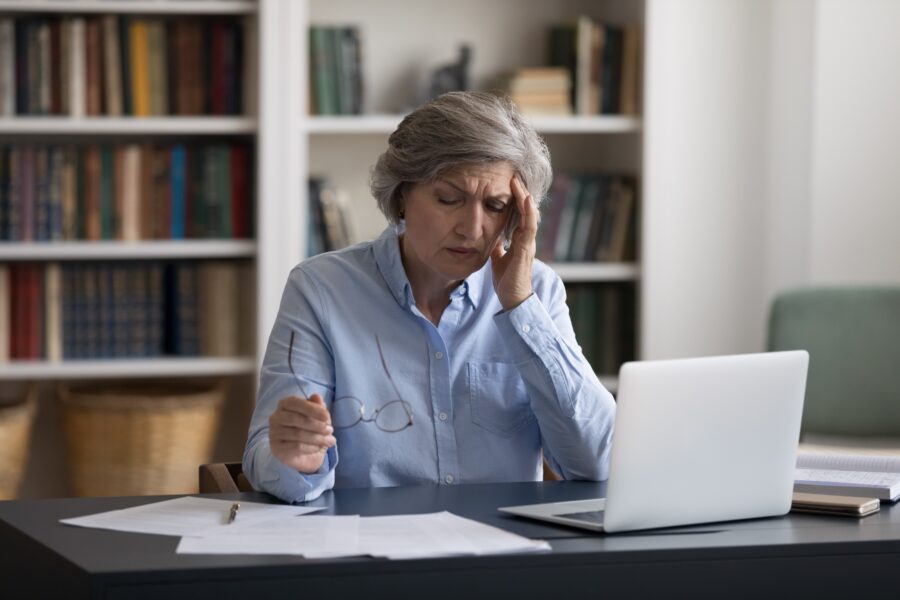
In its early stages, glaucoma often has no symptoms. This means that in some cases, the only way to diagnose it is by having your optic nerve examined and having the pressure of your eye measured by an optician.
It is thought that around half of all people in the UK with primary open angle glaucoma have not been diagnosed as they are typically unaware that they have it.
As the condition progresses, however, you may experience vision loss, particularly in your peripheral vision (your side vision).
Over time, this can lead to tunnel vision or even complete blindness if left untreated.
What’s the treatment for glaucoma?
The treatment for glaucoma depends on the type and severity of the condition. While there is no cure for glaucoma, the following are some common treatment options:
- Laser therapy: Laser procedures can be used to treat glaucoma by improving the drainage of fluid from the eye or reducing fluid production. Common laser treatments include selective laser trabeculoplasty, which opens up the drainage angle, and iridotomy, which creates a small hole in the iris to improve fluid flow.
- Eye drops: These drops help lower the fluid pressure inside the eye.
- Medication: In some cases, oral medications may be prescribed to lower the fluid pressure inside the eye or increase the fluid drainage.
- Surgery: In cases where medications and laser therapy are not effective or if the condition is severe, surgery may be recommended. There are different surgical options available, including trabeculectomy, where a new drainage channel is created, or the placement of drainage implants or shunts to facilitate fluid drainage.

Is glaucoma generic/hereditary?
There are some genetic factors which can contribute to an increased risk of developing certain types of glaucoma.
However, it's important to note that not all cases of glaucoma are directly inherited, and other factors such as age, ethnicity, and environmental factors can also play a role in its development.
If you have a family history of glaucoma, it's important to mention this to your optician. They will assess your risk factors and may recommend that you have more frequent eye tests to monitor or detect any signs of glaucoma early. Early detection and treatment are crucial in managing glaucoma and preserving vision.
Who is at risk for glaucoma?
Anyone can develop glaucoma, but certain factors can increase your risk. These include:
- Age: People over 60 are at increased risk for glaucoma.
- Family history: If someone in your family has had glaucoma, your risk may be higher.
- Race: people of African, Caribbean or Asian origin are at a higher risk.
- Medical conditions: Medical conditions like diabetes, high blood pressure, and heart disease can increase your risk of developing glaucoma.
What does glaucoma vision look like?
In the early stages, people with glaucoma may not notice any significant changes in their central vision, but they may experience blind spots or reduced peripheral vision.
Over time, without proper treatment, glaucoma can progress and cause tunnel vision, where the visual field narrows even further.
It's important to note that the exact visual changes can vary among individuals, and regular eye exams are crucial for early detection and treatment.

Can I still drive with glaucoma?
In the UK, you can still drive if:
- glaucoma only affects one of your eyes and
- you meet the visual standards for driving
You should meet the visual standards if you can:
- read a number plate from 20 metres away and
- have no double vision and
- have a normal field of vision in at least one eye
If you’re not sure if you meet these standards, your optician or GP will be able to give you some guidance.
If glaucoma affects both of your eyes, you must tell the DVLA.
For up-to-date guidance, visit the gov.uk website.

Is glaucoma a disability?
In some cases, glaucoma can be considered a disability if it significantly impacts a person's visual function and ability to perform daily activities.
However, eligibility for disability benefits, such as the Personal Independence Payment (PIP), vary by local council.
Contact your local disability services for guidance specific to your situation and location.
Is glaucoma painful?
In general, glaucoma itself is not painful.
Most forms of glaucoma develop gradually over time and are often asymptomatic in the early stages.
However, with acute angle-closure glaucoma (a less common type of glaucoma), can cause sudden symptoms such as severe eye pain, headaches, blurred vision, nausea, and vomiting. If you experience these symptoms, it's crucial to seek immediate medical attention, as acute angle-closure glaucoma is considered a medical emergency.
How can I reduce the risk of getting glaucoma?
There are several steps you can take to protect your vision and reduce your risk of glaucoma:
- Get regular eye exams: The only way to catch glaucoma in its early stages is through regular eye exams. It is recommended that people over 60 get an eye exam every two years and more frequently if you have other risk factors. Anyone over 40 with a family history of glaucoma is entitled to NHS funded eye examination in England and Wales.
- Manage underlying medical conditions: If you have medical conditions such as diabetes or high blood pressure, it is important to manage them properly to reduce your risk of glaucoma.
- Exercise regularly: Regular exercise can help improve blood flow to the optic nerve and may reduce your risk of glaucoma.
- Eat a healthy diet: A diet rich in fruits, vegetables, and omega-3 fatty acids has been shown in some studies to help protect against glaucoma.
- Quit smoking: Smoking has been linked to an increased risk of glaucoma, so quitting is important in protecting your vision.
- Take your medication as prescribed: If you have been diagnosed with glaucoma, it is important to take your medication as prescribed by your doctor to prevent further vision loss.

The insights and expertise shared in this article are brought to you by...
Matthew Burford BSc(Hons) Optometry MCOptom, Professional Services Manager at OutsideClinic
Matthew graduated from Aston University in 2004 before finding his passion for domiciliary eye care and joining OutsideClinic in 2005.