Blog post
Charles Bonnet Syndrome: What it is, Ways to Manage it and Risk Factors

Matthew Burford BSc(Hons) Optometry MCOptom - Domiciliary Optician and Professional Services Manager at OutsideClinic
8 minute read time
What is Charles Bonnet Syndrome?
Charles Bonnet Syndrome is a sight condition that causes people who have vision loss to see things that aren’t there – medically known as having a hallucination.

What causes Charles Bonnet Syndrome?
The exact cause of these hallucinations is not yet fully understood, but one of the main theories is that the brain generates hallucinations as a form of "phantom vision."
When individuals with vision loss experience a lack of visual stimulation, the brain may respond by generating visual experiences to compensate for the absence of incoming visual information.
Is Charles Bonnet Syndrome a sign of dementia?
In a nutshell, no. Many patients mistake Charles Bonnet Syndrome-related hallucinations for dementia or even a mental health issue, but Charles Bonnet Syndrome is an ocular condition.
Understandably, hallucinations can cause patients to worry that they have dementia or another condition, but generally if patients experience hallucinations without any other signs of dementia or mental illness, they will probably have Charles Bonnet Syndrome.
How common is it?
In the UK, around 100,000 people are thought to be affected by Charles Bonnet syndrome.
However, because Charles Bonnet Syndrome is not widely recognised and can be mistaken for other conditions, including dementia, misdiagnosis can occur. To avoid misdiagnosis, it's important for individuals experiencing hallucinations to consult with a healthcare professional who can evaluate their vision and rule out other potential causes of hallucinations.
Who is at risk of experiencing Charles Bonnet Syndrome?
Charles Bonnet syndrome is a condition that primarily affects individuals who have significant vision loss or impairment. It is more common in people who have conditions that cause visual deficits, such as macular degeneration, glaucoma, diabetic retinopathy, cataracts, or other eye diseases.
It’s estimated that up to half of all patients with macular degeneration will experience Charles Bonnet Syndrome at some point. Macular degeneration causes patches or ‘black spots’ in the vision, meaning the brain doesn’t receive as much information as it used to. With Charles Bonnet Syndrome, the brain works to fill in the gaps, creating patterns or hallucinations.
It can affect people of any age but generally, it occurs in patients later in life, which we most commonly see in our care home patients.
Can Charles Bonnet Syndrome be cured?
Currently, there isn’t a cure for Charles Bonnet Syndrome, but addressing the underlying eye condition, whether through cataract surgery, prescription eyewear, low vision aids or other appropriate treatments, can help.
A healthier visual system can lead to a reduction in the occurrence and severity of hallucinations.
How to manage visual hallucinations
- Simply reassuring the patient that hallucinations are signs of sight loss, not dementia or mental health issues, can be beneficial for patients, and reminds them that what they’re seeing isn’t real.
- Making sure that patients are familiar with their surroundings can also help them feel reassured when hallucinations make things look different.
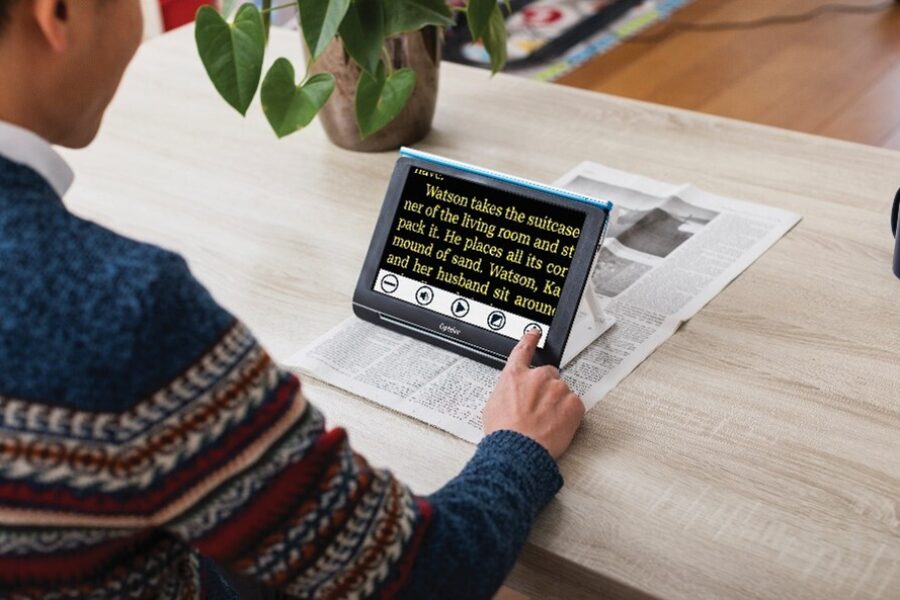
- Many people find that their hallucinations appear when they are sitting quietly without much occupying their mind. Engaging in activities that require focus and attention can help divert the mind from hallucinations. This might include reading, listening to music or participating in hobbies.
- Staying socially active and engaged in meaningful activities can help distract from hallucinations and maintain overall well-being.
- Making changes to the living environment can help to minimise the impact of hallucinations. Ensure good lighting, remove clutter and eliminate potential hazards to enhance safety.
- Let family members, friends and caregivers know about Charles Bonnet Syndrome and its hallucinations. Open communication can foster understanding and support from loved ones.
- Practicing relaxation techniques, such as deep breathing, progressive muscle relaxation or mindfulness meditation, can help reduce stress and anxiety related to hallucinations.
- Some people find that certain situations or environments trigger hallucinations. Identifying and avoiding these triggers, if possible, can be helpful.
- Utilise low vision aids and devices, such as magnifiers or CCTVs, to help maximise any remaining vision and perform daily tasks more easily.
- Keeping a journal of hallucinations can help individuals track patterns, triggers, and the frequency of these experiences. This information can be valuable when discussing the condition with healthcare professionals.
How is it diagnosed?
Diagnosing Charles Bonnet Syndrome can be somewhat complex because there isn't a single definitive test to confirm its presence.
The key to diagnosing Charles Bonnet Syndrome is the absence of other identifiable causes for the hallucinations. Once other potential causes have been ruled out, and there is a clear link between vision loss and hallucinations, a diagnosis is often made.
Is it hereditary?
While Charles Bonnet Syndrome itself is not hereditary, the underlying eye conditions that often lead to vision loss, and subsequently Charles Bonnet Syndrome, can have genetic components.
For example, conditions like macular degeneration, glaucoma or diabetes may have a genetic predisposition, meaning they can run in families.
How long does Charles Bonnet Syndrome last? Is it permanent?
The duration of Charles Bonnet syndrome and its associated visual hallucinations can vary widely from person to person. For some people the hallucinations may get less frequent over a few months, and they may eventually stop, but for others the condition may continue for years.
What does vision look like with Charles Bonnet Syndrome?
Patients can report anything from seeing children running across their bedrooms to spiders on the walls, colourful patterns or rooms changing shape.
Although not often scary in nature, hallucinations can be unsettling to experience – you’d undoubtedly get a fright from suddenly seeing a stranger or an animal appear in your home or seeing the room shift in shape or size.
They can also cause practical problems, with patients who see more complex hallucinations struggling with mobility or being unable to judge where they are or which direction they can walk in, depending on how distorted the vision becomes.

What should an individual do if they suspect they may be experiencing Charles Bonnet Syndrome?
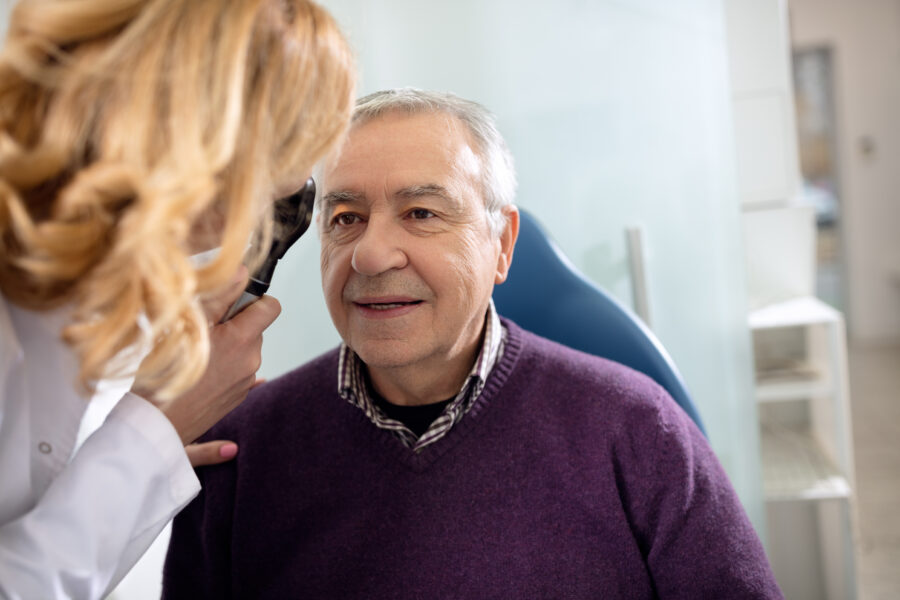
If you are concerned about Charles Bonnet Syndrome or think you or someone else may be suffering from it, it’s important to consult an Optometrist.
An eye test can help determine whether the hallucinations are related to an eye condition or if another cause is responsible. Treating or managing the underlying eye condition can help reduce the frequency and intensity of Charles Bonnet Syndrome hallucinations.
Our Optometrists here at OutsideClinic are trained to help eye health conditions affecting the older population, including Charles Bonnet Syndrome and macular degeneration, and can provide personalised advice and guidance.
We offer accessible and comprehensive eye tests conducted in the comfort of your own home. Our eye specialists are based all over the UK.
NHS funded at-home eye tests are available for eligible individuals who find it difficult to leave their home.
Check your eligibility for a sight test at home
If you would prefer the convenience of an at-home eye test, but you don't qualify for NHS funding, private home eye tests are available for £60.

By Matthew Burford BSc(Hons) Optometry MCOptom - Domiciliary Optician and Professional Services Manager at OutsideClinic
Matthew graduated from Aston University in 2004 with a degree in Optometry.